Understanding PGP: Causes, Symptoms, and Diagnostics
It’s an unfortunate reality that for many women, back pain is often dismissed as “just part of pregnancy.” While the shift in your body is massive and demanding, chronic or debilitating pain is not inevitable. At Hampstead Osteopathy, our goal is to help you understand the forces acting on your body so we can treat the cause, not just the symptom. Pelvic Girdle Pain (PGP) is a common condition that affects up to one in five pregnant women. It’s defined as pain felt in the pubic bone area and/or the joints at the back of the pelvis (the sacroiliac joints). Understanding what drives this pain is the first step toward effective relief.
The Two Primary Causes of PGP
PGP is typically the result of a powerful combination of two factors, both perfectly natural to pregnancy:
1. Hormonal Changes (The Structural Shift)
From the moment of conception, your body produces the hormone relaxin. This hormone does exactly what its name implies: it softens and relaxes the ligaments throughout your body, particularly those surrounding the pelvis. This relaxation is essential—it prepares the birth canal to expand for delivery. However, this loss of stability is also why PGP begins. The once-rigid joints of your pelvis become looser and less capable of handling the increasing mechanical stress of everyday movements.
2. Biomechanical Load Shifts (The Weight Distribution)
As your baby grows, the centre of gravity shifts drastically. The weight of the uterus pulls your pelvis forward, increasing the curve in your lower back (lordosis). This change forces the muscles of your lower back and glutes to work harder than ever just to keep you upright. The combination of loose, unstable ligaments and muscle imbalance puts undue stress on the sacroiliac joints, triggering inflammation and pain.
3. Identifying the Symptoms of PGP
PGP is distinct from general lower back pain. If you experience these specific symptoms, PGP is the likely culprit:
- Pubic Bone Pain: A sharp, shooting pain right over the front centre of your pelvis, often felt when lifting your leg, getting out of the car, or turning over in bed.
- Sacroiliac Joint Pain: Pain felt deep in the lower back, often favoring one side, and radiating into the buttocks or back of the thigh.
- Functional Limitations: Difficulty with weight-bearing activities, such as standing on one leg to put on trousers, climbing stairs, or walking long distances. You might notice an audible “clicking” or “grinding” sensation in the pelvis.
The Diagnostic Approach: Pinpointing the Source
As osteopaths, we don’t just rely on your symptoms; we use clinical observation and gentle diagnostic tests to isolate the specific joint or muscle responsible for your pain. During an assessment, we look for:
- Pelvic Symmetry: Observing whether your joints are loading and moving evenly.
- Muscle Strength & Imbalance: Assessing the stability and strength of your core, glutes, and hips to see where the body is compensating.
- Specific Movement Tests: Utilizing simple, safe movements (like the Active Straight Leg Raise Test) to determine exactly which joint is dysfunctional.
This detailed, manual assessment is why osteopathy is so effective. It allows us to create a treatment plan that targets the precise area of instability, providing fast, localized relief and helping you prepare safely for birth.
Sciatica During Pregnancy: True Nerve Compression vs. Muscle Referral
While PGP is centred on pelvic joint instability, Sciatica involves the largest nerve in the body and usually presents as a more intense, sharp pain travelling down the leg. In pregnancy, it can be confusing because the symptoms overlap with PGP. The key to effective treatment is distinguishing between true nerve compression and muscle referral.
True Nerve Compression (Less Common)
True sciatica occurs when the large sciatic nerve is irritated or compressed at its root in the lower spine. During pregnancy, this can be caused by:
- Disc Bulge/Herniation: Although less common in pregnancy, this remains a possibility.
- Uterine Pressure: In later trimesters, the sheer size and weight of the uterus can sometimes apply direct or indirect pressure on the nerve roots as they exit the spine or pass through the pelvis.
Symptoms of true nerve compression are often severe and localized: a sharp, electrical shooting pain, and sometimes noticeable numbness or tingling that follows a distinct nerve pathway down the back of the leg, often past the knee.
Pseudo-Sciatica and Piriformis Syndrome (Most Common)
The majority of sciatic-like pain in pregnancy is actually pseudo-sciatica, stemming from the over-tension of the Piriformis muscle in the buttock.
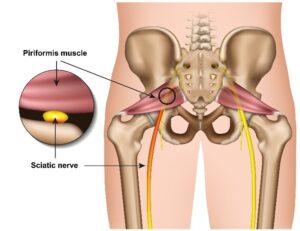
The piriformis muscle sits deep in the glutes and, in about 15% of the population, the sciatic nerve runs directly through it. The biomechanical changes of pregnancy—increased lordosis (swayback) and widening of the hips—cause the glutes and piriformis to tighten excessively in an effort to stabilize the newly unstable pelvis. This tightness compresses the nerve, causing pain that mimics true sciatica.
- Symptoms: This usually presents as a dull, deep ache or a burning sensation localized in the buttock and upper hamstring, rather than the severe, shooting pain of true nerve compression.
Crucial Red Flags (When to See Your GP or Midwife)
While osteopathy is highly effective for both PGP and pseudo-sciatica, certain symptoms require immediate medical attention before any manual therapy can proceed. These are rare but vital safety checks:
- Bilateral Symptoms: Sciatica affecting both legs simultaneously.
- Foot Drop: The inability to lift the front part of the foot.
- Sudden Loss of Function: Any new and sudden weakness or loss of sensation in the legs.
- Bladder/Bowel Changes: Loss of bladder or bowel control, or numbness around the saddle area (inner thighs/groin).
If you experience any of these red flags, contact your GP or midwife immediately. For all other sciatica and PGP symptoms, osteopathic assessment is the safest and most effective first step.
The Osteopathic Treatment Approach for PGP (First Trimester Safety)
Once a patient presents with symptoms of PGP or pseudo-sciatica, the primary aim of osteopathic treatment is to reduce pain and restore balance without adding further stress to the already unstable pelvis. We always work within the comfort level of the patient, prioritizing safety above all else, especially during the crucial first trimester.
1. Gentle Joint Mobilization, Not Manipulation
Because the ligaments are already softened by relaxin, any high-velocity, low-amplitude (HVLA) manipulation techniques are avoided near the pelvis. Instead, we use gentle, sustained articulation and mobilization techniques to encourage correct alignment.
- PGP Focus: We gently articulate the sacroiliac and pubic symphysis joints to restore functional movement within the available range. This reduces painful friction without increasing overall joint laxity.
- The Goal: We are not “clicking” the joint back into place; we are persuading the surrounding musculature to allow the pelvis to settle into a more symmetrical and stable position.
2. Targeted Soft Tissue Therapy and Muscle Balancing
The pain of PGP is often intensified by the muscles surrounding the pelvis—the glutes, hip flexors, and lower back extensors—working overtime to compensate for the joint instability.
- Addressing Pseudo-Sciatica: We apply specific, deep soft tissue techniques (like Muscle Energy Technique or trigger point release) to the Piriformis muscle and the gluteal complex. Relieving this tension is the fastest way to decompress the sciatic nerve and alleviate the burning sensation associated with pseudo-sciatica.
- Restoring Balance: We focus on releasing tight, compensating muscles while gently activating deep stabilizing muscles that have been switched off by the postural changes.
3. Safe Treatment Positions in the Clinic
Patient comfort and safety are paramount in all stages of pregnancy.
- First Trimester and Beyond: Patients are typically treated in side-lying positions, or sometimes semi-reclined using specialist pregnancy cushions and supports that relieve all pressure on the abdomen. This ensures the patient is fully relaxed and protects the growing baby.
- Prioritizing Communication: Every treatment begins with a detailed check-in to assess current pain levels, energy, and comfort with the treatment position. If a position is uncomfortable, we change it immediately.
This targeted, gentle approach works to interrupt the pain cycle, allowing the joint-supporting muscles to relax and stabilize the pelvis for the remaining months of pregnancy.
Specialized Treatment: Osteopathy for Later Stages of Pregnancy
As you move into the second and third trimesters, the focus of osteopathic care often shifts as your body’s demands change dramatically. While we continue to manage PGP and sciatica, new symptoms frequently emerge due to the significant increase in internal pressure and the sheer size of the baby.
Addressing Upper Body Strain: Rib Pain and Breathlessness
In the final stages of pregnancy, the expansion of the uterus pushes upwards, often causing the ribs to flare and placing sustained tension on the diaphragm and the intercostal muscles. This can lead to:
- Rib Pain: Sharp, localized pain, often around the front lower ribs, which can feel tight or restricted.
- Breathlessness: The diaphragm’s inability to move fully due to mechanical restriction.
Our treatment approach expands upward to address these areas. We use gentle thoracic and rib cage articulation to restore mobility, ease muscle tension around the rib attachments, and encourage the diaphragm to function more efficiently. This often results in an immediate feeling of relief and improved breathing capacity.
Pelvic Preparation for Labour
As you approach your due date, osteopathic treatment focuses on ensuring the pelvis is as mobile and balanced as possible to facilitate an optimal labour experience.
- Sacral Mobility: We ensure the sacrum (the triangular bone at the base of the spine) is free from restriction. The sacrum needs to be able to move and extend during birth to allow the widest possible passage for the baby. Gentle, sustained release techniques are applied to the muscles and ligaments attached to the sacrum.
- Optimal Foetal Positioning: While osteopathy cannot “turn” a baby, ensuring the mother’s pelvis and lower back are completely balanced helps remove any unnecessary physical restrictions. This encourages the baby to settle into the best possible position for delivery.
Positioning and Safety
Throughout the later stages, we utilize comfortable and secure positioning. Side-lying remains the most common and safest position, often combined with pillows that support the entire spine, hips, and abdomen, making the session comfortable and relaxing. Our manual techniques remain entirely gentle, focusing on soft tissue balance and low-force mobilization.
At-Home Management and Self-Care
The effectiveness of your osteopathic treatment relies heavily on the work you do at home between appointments. We empower you with safe, practical self-management strategies designed to stabilize the pelvis, maintain the benefits of treatment, and relieve daily muscular tension.
1. Mastering Safe Movement and Ergonomics
The majority of PGP flares occur during simple, daily tasks that load the pelvis unevenly.
- Getting Out of Bed (The Log-Roll): Never swing your legs out one at a time. To get out of bed, roll onto your side (keeping your knees together), and then push yourself up to sitting using your arms. This maintains stability in the pubic symphysis.
- Entering and Exiting the Car (The Swivel): Always enter or exit the car with your knees and feet together. Sit on the edge of the seat first, and swivel your entire body together. This prevents the shearing force that triggers pain.
- Standing Posture: When standing for long periods (e.g., washing dishes), stand with your weight equally distributed. Avoid resting weight on one hip, which exaggerates pelvic instability and increases pain.
2. The Best Sleeping Position
Sleep can be a major trigger for pain. The goal is to keep the pelvis as neutral as possible throughout the night:
- Side-Lying is Best: Always sleep on your side (the left side is often preferred for circulation).
- The Pillow Sandwich: Place a supportive pillow between your knees, and another smaller pillow between your ankles. This prevents the upper leg from rotating and dragging the pelvis, ensuring the pubic symphysis remains aligned.
- Wedge Support: Some women find placing a small wedge or cushion under the abdomen can also help support the weight and take pressure off the lower back.
3. Gentle Movement for Pain Relief
We prescribe movements that improve mobility without introducing instability. Avoid exercises that require standing on one leg or wide lunges unless specifically advised by your practitioner.
- Pelvic Tilts (Rocking): This is your primary exercise. On all fours or lying on your back (if comfortable), gently tilt your pelvis, rocking your lower back from slightly arched to flat. This encourages fluid movement in the sacrum and gently releases tension from the lower back and abdomen. Perform this 10-12 times slowly, several times a day .
- Gentle Hip Circles: While standing and holding onto a stable chair, gently circle your hips clockwise and anti-clockwise. Keep the movement small and slow; this helps lubricate the hip joints and maintain mobility without straining the ligaments.
- The Cat-Cow Modification: On hands and knees, gently arch and round your back. Crucially, keep the movement smooth and small, and stop before feeling any pull or strain on the pubic bone. This is excellent for spinal fluid exchange and movement.
By consistently applying these techniques, you become an active participant in your care, stabilizing your joints and managing your symptoms effectively between visits.
Postpartum Recovery: Addressing Diastasis Recti and Core Strength
The pregnancy journey doesn’t end with delivery; the nine months after birth are just as crucial for physical recovery. While the mechanical load is gone, hormonal changes persist, and a new set of physical demands—feeding, lifting, and carrying a baby—can introduce new strains.
Navigating the Postpartum Body
Relaxin hormone levels can remain elevated for several months, especially if breastfeeding, meaning the joints you struggled with during pregnancy (PGP) remain vulnerable. Postpartum care is about addressing the lingering instability and treating the new muscular pains associated with being a new parent (often neck and upper back issues from feeding positions).
Understanding Diastasis Recti (DR)
One of the most common issues is Diastasis Recti (DR), a widening of the gap between the two sides of the outermost abdominal muscle (rectus abdominis). This happens as the connective tissue (linea alba) stretches to accommodate the growing baby.
- Osteopathic Role: We assess the degree of separation and, critically, the integrity of the deeper core muscles. We don’t ‘fix’ the gap; instead, we help re-establish proper function and stability around the core.
- The Key to Recovery: Safe, progressive rehabilitation. High-impact exercises and traditional crunches are strictly forbidden in early recovery as they can worsen DR. We guide you toward safe breathing and deep core activation techniques that help reconnect the core safely.
Treating New Parental Strains
- Upper Back and Neck: Manual therapy focuses on relieving the sustained tension from looking down during feeding or carrying the baby one-sidedly. Releasing the neck, thoracic spine, and shoulder girdle can dramatically reduce tension headaches and chronic stiffness.
- Guidance on Safe Lifting: Providing ergonomic advice on lifting car seats, pushchairs, and the baby itself is paramount to preventing a return of lower back pain or PGP.
Why Choose a Registered Osteopath
When dealing with the complex biomechanical changes of pregnancy, expertise and safety are non-negotiable. Your body deserves the highest level of regulated care.
- GOsC Registration: All treatments at Hampstead Osteopathy are provided by Ben Posen, a fully registered member of the General Osteopathic Council (GOsC Number 6848) since 2008. This registration ensures adherence to the highest standards of safety, professional conduct, and clinical competence, confirming you are treated by a properly qualified and insured specialist.
- Specialist Focus: Our practice is founded on years of experience focusing on complex musculoskeletal issues, with a dedicated specialism in the biomechanics of pregnancy and postpartum recovery.
The Holistic, Safe Approach
Osteopathy is unique in its holistic, hands-on approach. We don’t just treat the site of pain (e.g., the pubic bone); we look at the entire system—the diaphragm, the thoracic spine, the hips—to find the root cause of the imbalance. For expectant and new mothers, this commitment to safe, gentle, and drug-free treatment is precisely why osteopathy is so highly recommended by midwives and GPs.
Conclusion and Next Steps
Persistent pain during or after pregnancy is not something you simply have to endure. This guide has shown that relief is possible through understanding and expert, hands-on care.
If you are struggling with PGP, sciatica, or postpartum strains, taking the first step towards personalized care is crucial. We offer tailored treatment plans designed not only to eliminate pain but to empower you with the knowledge and stability needed for a comfortable, strong pregnancy and recovery.
Take the next step towards pain-free pregnancy. Book your consultation with Hampstead Osteopathy today.

